What is Perimenopause? And how to improve potential disturbed sleep
When I first encountered Perimenopause it demanded the swift footedness of a wild panther. In my case, I wasn’t so lucky, and a large fluffy pillow smacked me right in the head. I had managed to irritate her this evening by mentioning that she looked ‘redder’ than usual. This was her toeing the cusp of perimenopause and the ‘redness’ were hot flashes that would come and go over the months along with irregular periods and sleepless nights, making everyone at home miserable.
Perimenopause, recognized as the menopausal transition, encapsulates the intricate hormonal and reproductive changes that precede menopause. Commencing typically in the 40s, Perimenopause extends over multiple years, culminating in menopause, officially designated after 12 consecutive months without menstruation. This reproductive chronicle highlights the physiological shifts signaling the culmination of a woman’s fertile years.
“Menopausal transition,” is a natural part of aging that signals the approach of menopause and a close on being able to give birth thereafter. While perimenopause brings about various changes in the body, one aspect that significantly impacts women during this time is sleep. Let’s try and understand the intricacies of perimenopause and its profound effects on sleep while exploring the science behind this phase in a woman’s life while creating the space for her to understand her body better, feel loved and appreciated.
What are somethings that can put you into an early menopause?
Environmental factors have changed nowadays and there are a few reasons why one can step into peri-menopause early:
- Faster ageing because of environmental reasons, staying in areas where there is excessive pollution, hormones in dairy etc
- Family history or genetic predisposition
- Cancer treatment
- If one has had their uterus removed
Understanding the Transition:
Perimenopause typically begins in a woman’s 40s but can start earlier for some. It’s characterized by fluctuations in hormone levels, specifically estrogen and progesterone, as the body gradually prepares for the cessation of menstruation. These hormonal shifts can manifest in a myriad of symptoms, from hot flashes, irregular periods and mood swings to changes in sleep patterns.
Association of Professional Sleep Societies journal says that “Vasomotor episodes (i.e., hot flashes) are variable in severity in perimenopausal women. However, they might serve as an indicator of central nervous system vulnerability to the effects of changing gonadal hormones, creating instability that is manifested as sleep and perhaps temperature pattern changes, independently or in concert.” For many women, the onset of perimenopause can bring about sleep disturbances that were once unfamiliar. The reasons behind these disruptions are multifaceted and interconnected, involving both physical and hormonal changes. As sleep becomes a precious commodity, understanding the nuances of perimenopause becomes essential for navigating this transformative phase with grace and support from family and alternative therapies.
Unlocking the Impact of Perimenopause: Embracing Transformations
1. Irresistibly Irregular Periods: Say hello to the unpredictability of perimenopause with irregular periods, a quirky dance of varying lengths and flows. Is it early or late perimenopause? Let your cycles spill the secrets.
2. Hot Flashes and Midnight Musings: Brace yourself for the infamous hot flashes – those unexpected bursts of warmth stealing the spotlight. And as if that’s not enough, the sleep arena becomes a wild card, with or without the fiery flashes.
3. Mood Roller Coaster:Get ready for a mood extravaganza! Mood swings, a touch of irritability, or a flirtation with the blues might make an entrance. Blame it on sleep disturbances or chalk it up to perimenopausal flair.
4. Bladder Ballet and Vaginal Variations: A duo of challenges descends – vaginal dryness and bladder whimsies. Intimacy may get a makeover, and the urge to visit the bathroom might strike at unexpected moments.
5. Fertility’s Subtle Fade: Ovulation takes a leisurely stroll, signaling a decrease in fertility. Yet, surprise – the chance of pregnancy persists until the curtain falls on periods for a solid 12 months.
6. Passion’s Plot Twist: Sexual function may rewrite some chapters during perimenopause. But fear not, the saga of satisfaction in intimate escapades typically endures the hormonal twists.
7. Bone Ballet: A silent performance unfolds as estrogen takes its bow, triggering accelerated bone loss. Beware the osteoporosis waltz, where bones may become more delicate dancers.
8. Cholesterol Symphony: Hormonal shifts compose a new tune for cholesterol levels. LDL cholesterol might play a daring solo, while HDL cholesterol takes a subtle backseat, adding a note of heart health intrigue.
Hormonal Flux and Sleep Architecture with alternative medicine:
Delving into the intricacies of perimenopause requires a closer look at the hormonal fluctuations that define this stage. Estrogen, a key player in the menstrual cycle, experiences erratic surges and declines during perimenopause. This rollercoaster ride can disrupt the delicate balance of sleep-regulating hormones, impacting the overall sleep architecture. There are numerous ways to support this change by increasing intake of multivitamins, adding magnesium to both your diet and via supplementation before bedtime, reducing stress through breathwork and meditation whilst using massages with essential oils as a daily ritual to calm and soothe the nerves.
Estrogen is closely tied to serotonin and melatonin production, neurotransmitters essential for regulating mood and sleep. As estrogen levels fluctuate, so does the delicate equilibrium of these neurotransmitters, contributing to insomnia, night sweats, and restless nights for many women in perimenopause. The National Certificate for Biotechnology Information released an article with the findings that “Aromatherapy, massage, yoga, and acupuncture, as well as some dietary and herbal supplements improved psychological symptoms during menopause.” Complementary medicine in many cases are an effective way to transition into a new stage of life with minimum discomfort.
Progesterone, another vital hormone, also plays a role in sleep regulation. During perimenopause, progesterone levels may decline, further complicating the sleep landscape. The interplay between estrogen and progesterone during this transitional phase can create a perfect storm for sleep disturbances.
“Reduced sleep efficiency was more evident in women who reported experiencing hot flashes, i.e. were more symptomatic, than those not.” Many women have found that perimenopausal symptoms can be reduced through exercise, eating right and sleeping well. The other effects of perimenopause during this stage can include but are not limited to are ,breast tenderness, and decreased sex drive. This stage typically lasts 4-8 years and occurs in the middle to late 40s, although it can begin a decade earlier. It is a good idea to stay connected to your health care provider and continue to explore holistic medicine, Ayurveda and even supplementation such as COQ10, Magnesium, Primrose oil, Omega 3 fatty acids and other supportive additions that can help you maintain your bone health, keep you at a health weight, keep excess fat off and manage your energy levels in a balanced way.
The Heat Factor: Understanding the Correlation Between Hormonal Shifts and Nocturnal Temperature Fluctuations
The journey through perimenopause is often accompanied by a unique and challenging phenomenon – night sweats and hot flashes. These nocturnal disruptions can turn what was once a peaceful night’s sleep into a series of restless moments, leaving women fatigued and frustrated. The root of this disturbance lies in the hormonal fluctuations characteristic of perimenopause, particularly the erratic changes in estrogen levels. As estrogen waxes and wanes, it exerts a profound influence on the body’s internal thermostat, triggering sudden bursts of heat. These hot flashes, often experienced as intense warmth spreading across the face and upper body, are frequently followed by the body’s attempt to cool down through night sweats, leading to damp sheets and an overall discomfort that disrupts the natural sleep cycle.
To comprehend the intricacies of night sweats and hot flashes during perimenopause, it’s crucial to explore the “heat factor” and its connection to hormonal shifts. Estrogen, the primary player in the menopausal transition, plays a central role in regulating the body’s temperature. As estrogen levels decline, the hypothalamus, the body’s thermostat, can become more sensitive to slight changes, leading to exaggerated responses like hot flashes. Additionally, these hormonal shifts impact the body’s ability to regulate melatonin, the sleep hormone, further complicating the relationship between hormonal changes and temperature fluctuations. Recognizing this correlation provides a foundation for developing effective coping strategies that address both the physiological and environmental aspects of managing night sweats, ultimately fostering better sleep hygiene during perimenopause.
Sleep Disorders Amplified: Insomnia and Sleep Apnea
As women navigate the intricate terrain of perimenopause, they often find themselves contending with a double-edged sword in the realm of sleep – the tandem challenges of insomnia and sleep apnea. Insomnia, characterized by difficulty falling or staying asleep, becomes a prevalent companion during this transitional phase. The hormonal fluctuations, particularly the erratic changes in estrogen and progesterone, contribute significantly to the increased prevalence of insomnia. Fluctuating hormone levels can disrupt the delicate balance of neurotransmitters, such as serotonin and melatonin, which play a crucial role in the regulation of sleep patterns. Additionally, the psychological aspects of perimenopause, including heightened stress and anxiety, can further exacerbate insomnia symptoms, leading to a challenging cycle of sleep disturbances for many women.
Simultaneously, the emergence of sleep apnea adds another layer of complexity to the perimenopausal sleep landscape. Sleep apnea is characterized by interruptions in breathing during sleep, often accompanied by loud snoring and sudden awakenings. While sleep apnea can affect individuals of any age or gender, perimenopausal women face an increased risk due to factors such as hormonal changes, weight gain, and alterations in upper airway anatomy. The implications of sleep apnea for women in perimenopause are profound, as untreated sleep apnea not only contributes to poor sleep quality but also poses potential risks to cardiovascular health. Understanding and addressing these sleep disorders becomes imperative for women navigating perimenopause, emphasizing the need for comprehensive strategies that address both the hormonal and physiological aspects of sleep.
Circadian Rhythm Shifts and Chronotype Alterations
The journey through perimenopause brings about not only hormonal fluctuations but also subtle yet impactful shifts in the body’s internal clock – the circadian rhythm. Investigating these rhythmic imbalances reveals the intricate dance between hormones and the natural ebb and flow of the sleep-wake cycle during this transitional phase. The circadian rhythm, a finely tuned 24-hour biological cycle, regulates various bodily functions, including sleep, and is influenced by external cues such as light and temperature. As women traverse perimenopause, hormonal changes, particularly the decline in estrogen, can disrupt this delicate balance. The result is often a disconcerting misalignment between the body’s natural rhythm and external factors, leading to difficulties falling asleep, staying asleep, or waking up too early.
In tandem with circadian rhythm shifts, perimenopause may also cast a subtle influence on an individual’s chronotype – their natural sleep-wake preferences. Understanding how perimenopause influences these chronotype changes is pivotal for tailoring sleep strategies to individual needs. Some women may find themselves naturally gravitating towards earlier bedtimes and waking up with the sunrise, while others may experience a shift towards becoming “night owls.” These changes in chronotype can be attributed to hormonal fluctuations and may impact not only the timing of sleep but also overall sleep quality. Acknowledging and adapting to these alterations in chronotype during perimenopause empowers women to optimize their sleep patterns and enhance their overall well-being during this transformative phase.
Psychological Factors: Stress, Anxiety, and Depression and Perimenopause Sleep Issues
Embarking on the journey through perimenopause, women often find themselves navigating not only physical changes but also a complex interplay of psychological factors that can profoundly impact sleep quality. At the forefront of these factors are stress, anxiety, and depression, which intricately weave into the fabric of perimenopausal sleep challenges.
The relationship between stress and sleep during perimenopause is akin to a delicate dance, where each partner influences the other in a bidirectional manner. The tumultuous hormonal changes characteristic of perimenopause can act as stressors on the body, disrupting the natural sleep-wake cycle. Simultaneously, heightened stress levels can exacerbate hormonal imbalances, creating a challenging loop that interferes with the ability to achieve restorative sleep.
Understanding this intricate nexus is essential for women navigating perimenopause, as managing stress becomes not just a means of promoting mental well-being but also a key strategy for addressing sleep disturbances. It is a great idea to reach out to a professional or a coach for counseling, therapy and meditation and breathwork practices to keep one’s mental and physical health in shape.
Unraveling Anxiety and Depression: Exploring the Psychological Factors Contributing to Sleep Disturbances
Anxiety and depression, prevalent psychological factors during perimenopause, cast a shadow over the realm of sleep. Anxiety, often fueled by the uncertainties and changes associated with this life stage, can manifest as intrusive thoughts and restlessness, impeding the journey into a restful night’s sleep. Depression, with its pervasive influence on mood and energy levels, can lead to persistent feelings of fatigue and lethargy, affecting both the initiation and maintenance of sleep. Unraveling these psychological factors is a crucial step in comprehending the intricacies of perimenopausal sleep disturbances. By exploring the multifaceted connection between psychological well-being and sleep, women can tailor holistic strategies to address not only the physical aspects of perimenopause but also the emotional landscape, fostering a more comprehensive approach to reclaiming restful nights.
Practical Tips for Managing Perimenopausal Sleep Disruptions:
Amidst the intricacies of perimenopause, adopting targeted lifestyle modifications can be a powerful ally in reclaiming restful nights. Two key pillars in this endeavor are nutrition and sleep hygiene, as well as exercise and relaxation techniques.
During perimenopause, estrogen’s erratic levels disturb neurotransmitters, affecting sleep quality. Progesterone, known for its calming influence, becomes pivotal, and its decline may trigger heightened anxiety and restless sleep. Melatonin, the “sleep hormone,” faces disruptions influenced by estrogen fluctuations, contributing to difficulties falling asleep. Recognizing the nuanced interplay of these hormones empowers women to tailor strategies for improved sleep during this transitional phase. Targeted interventions, such as lifestyle adjustments and possibly hormone replacement therapy, based on individual needs, can address perimenopausal sleep challenges, fostering a more restful and resilient sleep experience amid the hormonal intricacies of this transformative stage.
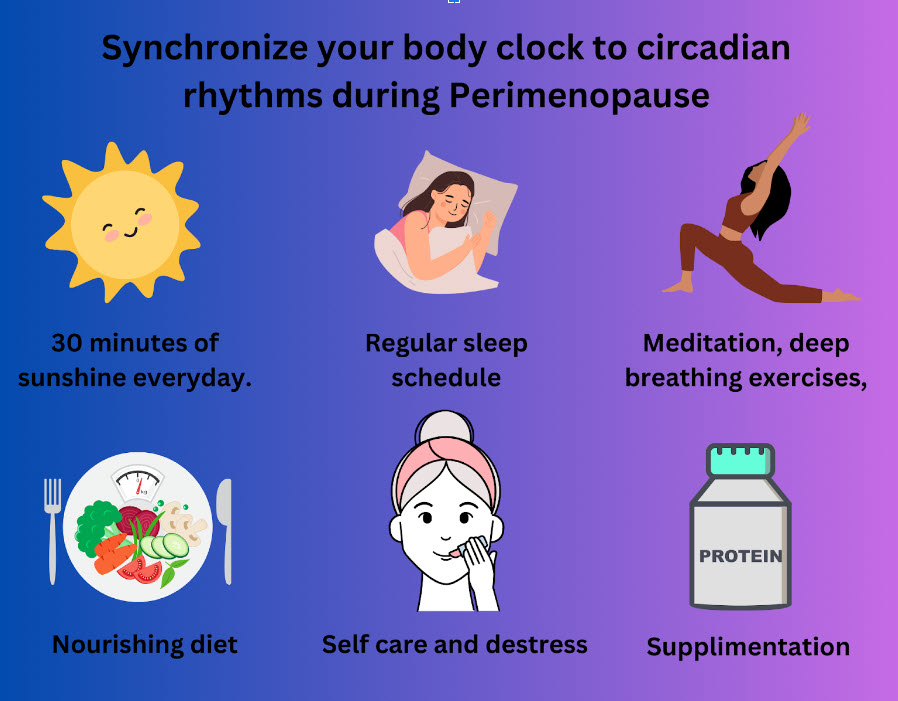
A regular routine is an effective way to synchronize your body clock to circadian rhythms.
- Make sure you get at least 30 minutes of sunshine everyday. Make sure the sun falls directly on your skin.
- Creating a regular sleep schedule reinforces the body’s natural circadian rhythm, promoting better sleep quality. Have a gradual winddown routine that can bring you into a calm and relaxed frame of mind.
- Prioritize Relaxation Techniques: Incorporating relaxation practices such as meditation, deep breathing exercises, or yoga can help manage stress and improve sleep.
- Maintain a Cool Sleeping Environment: Night sweats are common during perimenopause, so keeping the bedroom cool and comfortable can mitigate discomfort and support better sleep.
- Eating a nourishing diet- that can help balance vitamins and minerals in the body.
- Symptom Relief Strategies
a) Consider Hormone Replacement Therapy (HRT): This is a route often taken by many women who have extreme symptoms but may possibly have side effects. Consult with a healthcare professional to explore the potential benefits of hormone replacement therapy in managing perimenopausal symptoms, including sleep disturbances.
It is always advisable to exhaust all alternative therapies before resorting to any therapies that can impact your hormones or create further symptoms that can bring discomfort.
Healthcare providers offer treatments to ease perimenopausal options may include:
b) Antidepressants: Address mood swings and depression
c) Birth Control Pills: Stabilize hormone levels, alleviating symptoms.
d) Estrogen Therapy: Balances estrogen levels through creams, gels, patches, or pills.\
e)Gabapentin: Originally a seizure medication, it also relieves hot flashes.
f) Vaginal Creams: Prescribed or over-the-counter options to reduce pain during intercourse and relieve dryness.
Nutrition and Sleep Hygiene: Implementing Dietary and Lifestyle Changes to Support Improved Sleep during perimenopause
Crafting a sleep-friendly diet and lifestyle is pivotal during perimenopause. Certain foods, such as those rich in tryptophan (found in certain meats, nuts, and seeds), can promote the production of sleep-inducing neurotransmitters like serotonin. Limiting caffeine intake, particularly in the afternoon and evening, helps mitigate the risk of disrupting the natural sleep-wake cycle. Additionally, establishing a consistent sleep routine, with regular bedtimes and wake-up times, reinforces the body’s internal clock. Creating a calming pre-sleep ritual, such as reading or gentle stretching, can signal to the body that it’s time to wind down. By combining these dietary and lifestyle changes, women can foster an environment conducive to improved sleep quality during the perimenopausal journey.
Physical activity and stress-reduction practices play pivotal roles in enhancing sleep quality during perimenopause. Regular exercise, whether through aerobic activities or calming practices like yoga, not only promotes physical health but can also positively impact sleep patterns. Engaging in exercise earlier in the day helps regulate energy levels and contributes to a more restful night. Additionally, incorporating relaxation techniques such as deep breathing exercises, meditation, or mindfulness practices can mitigate stress and anxiety, common culprits behind perimenopause sleep disturbances. By intertwining physical activity and stress-reduction practices into the daily routine, women can cultivate a holistic approach to better sleep, fostering overall well-being during this transformative phase of life.
Medical Interventions: Exploring Pharmacological and Non-Pharmacological Treatments for Perimenopausal Sleep Problems
When lifestyle modifications alone may not suffice, medical interventions offer a spectrum of options to address perimenopausal sleep problems. Pharmacological treatments, such as hormone replacement therapy (HRT), can help regulate hormonal imbalances, offering relief from symptoms that disrupt sleep. However, it’s essential to weigh the potential benefits against the risks and consult with a healthcare professional to determine the most suitable approach.
Non-pharmacological treatments also play a significant role in managing perimenopause sleep issues. Some women may benefit from supplements like melatonin or herbal remedies known for their sleep-inducing properties- Ashwagangha and peppermint essential oils are frequently used.Chamomile tea made from flowers is another one. Behavioral therapies, such as sleep restriction and stimulus control, may be employed to reshape sleep patterns without relying on medication. The multifaceted nature of perimenopausal sleep disturbances often necessitates a personalized approach, with healthcare providers tailoring interventions to individual needs and preferences.
The Role of Cognitive-Behavioral Therapy: Understanding How Therapeutic Interventions Can Positively Impact Sleep
Cognitive-Behavioral Therapy for Insomnia (CBT-I) stands out as a particularly effective non-pharmacological approach for improving sleep quality during perimenopause. This therapeutic intervention addresses the cognitive and behavioral aspects contributing to sleep difficulties. CBT-I encompasses various strategies, including cognitive restructuring to modify negative thought patterns about sleep, sleep hygiene education, and stimulus control to strengthen the association between the bedroom and restful sleep.
One of the strengths of CBT-I is its focus on sustainable, long-term changes in sleep habits. It empowers individuals to develop skills that extend beyond the therapy sessions, promoting lasting improvements in sleep quality. Working with a trained therapist allows women to explore the root causes of their sleep disturbances and develop personalized strategies to overcome them. As a well-established and evidence-based approach, CBT-I offers a valuable tool in the arsenal against perimenopause sleep problems, emphasizing the importance of addressing the psychological aspects intertwined with hormonal changes during this transformative phase.
Yoga Nidra during the perimenopause stage helps one fall asleep faster and gives you deeper rest. You can find more on Sleep Dragon’s yoga nidra and non sleep deep rest techniques here.
Navigating Perimenopausal Sleep Challenge
The perimenopausal journey brings with it a unique set of challenges for women, particularly in the realm of sleep. From hormonal fluctuations to psychological factors, understanding these intricacies is key to developing effective strategies for a restful night’s sleep. By acknowledging the interplay of hormones, addressing specific symptoms like night sweats, and adopting holistic lifestyle changes, women can proactively manage perimenopause sleep issues. Seeking professional guidance and staying informed about evolving research in this field further empower individuals to navigate this transitional phase with resilience. Ultimately, fostering harmony in the night during perimenopause involves a multidimensional approach that encompasses hormonal balance, lifestyle modifications, and a proactive mindset towards well-being.